
Sleeping, including position, may affect your risk of developing neurodegenerative diseases
We all know that sleep is super important for our health, but did you know that whether you sleep on your back, front or side, as well as the quality of your sleep, can have an impact on your propensity to develop certain neurodegenerative diseases, for example, motor neuron disease (MND)?
A recent study using rodents found that side-sleeping, rather than supine or prone, may be a better position to avoid developing diseases like MND (also called amyotrophic lateral sclerosis (ALS) and Lou Gehrig’s disease).
Other neurodegenerative diseases, like Parkinson’s disease, Alzheimer’s and multiple sclerosis, share many similarities with ALS/MND1, even though their clinical symptoms and disease progression may look very different. These similarities include:
- Increased incidence with age
- Progressive damage to cells and nervous system connections
- Adverse impact on mobility, coordination, strength, sensation, and cognition
- Gradual loss of brain tissue
- Accumulation of waste proteins in the brain.
Waste removal in the brain
The glymphatic system, a recently discovered macroscopic waste clearance system for the brain, plays a critical role in these conditions. It appears to use a unique system of perivascular channels to promote efficient elimination of soluble proteins and metabolites from the central nervous system. Besides waste elimination, the glymphatic system may help distribute non-waste compounds, such as glucose, lipids and amino acids 2, 3. It is believed that the glymphatic waste system feeds into the lymphatic system, although the mechanism is not clearly understood. The glymphatic system has been well studied in rodents and the current hypothesis, based on research, observation and conjecture, is that the human system is similar.
The biological differences between rodents and humans include:
- Heart rate: humans at 60 to 70 beats per minute whereas rats sit at around 300 and mice at around 500
- Cerebrospinal fluid formation rate: in rats has been reported to be 300-fold that of humans
- Cerebrospinal fluid turnover rate: in young normal rat brains is 11 volumes/day, whereas in the larger human brain turnover rate is 4 times/day.
Source: Benveniste, Helene et al. “The Glymphatic System and Waste Clearance with Brain Aging: A Review.” Gerontology vol. 65,2 (2019): 106-119. doi:10.1159/000490349
Faster glymphatic transport and waste clearance during sleep in rodents was associated with enhanced clearance of soluble beta-amyloid from brain tissue, a protein that has been implicated in neurodegenerative diseases. Several new studies correlating beta-amyloid levels in cerebrospinal fluid and/or the brain of humans with changes in sleep architecture and hours of arousal have recently emerged supporting the presence of a glymphatic system in the human brain.
How can we improve glymphatic function whilst awake?5
- Exercise is beneficial. More information on the form of exercise will be covered in a separate article.
- Omega-3, found in marine-based fish, considered beneficial to health, appears to specifically reduce the risk of neurodegenerative diseases. New research shows these benefits may be partly due to the positive effect of Omega-3 on glymphatic function.
- Moderate consumption of alcohol improves waste clearance. In mice studies, both short and long-term exposure to small amounts of alcohol were shown to boost glymphatic function while high doses of alcohol had the opposite effect.
These small lifestyle changes can improve brain waste clearance and so reduce the risk of neurodegenerative disease.
How can we improve glymphatic function whilst sleeping?
Research has shown a single night without sleep (or just with disrupted sleep) results in increased accumulation of toxic waste protein in the brain4.
- Maximise slow wave sleep – This is when the glymphatic system is most active. Sleep therapies that enhance this phase may prove to be particularly beneficial for preventing diseases like ALS/MND.
- Sleep position is also thought to affect glymphatic clearance with research conducted in rodents demonstrating superior clearance in the lateral (or side-sleeping) position, compared to either supine (on the back) or prone (front-lying) positions. The reasons for this are not yet fully understood but possibly relate to the effects of gravity, compression and stretching of tissue5.
When we sleep, we cycle through each of the stages as shown in the graph below. Cycles earlier in the night tend to have more deep sleep while later cycles have a higher proportion of REM or rapid eye movement sleep. By the final cycle, the deep sleep stage may be skipped altogether.
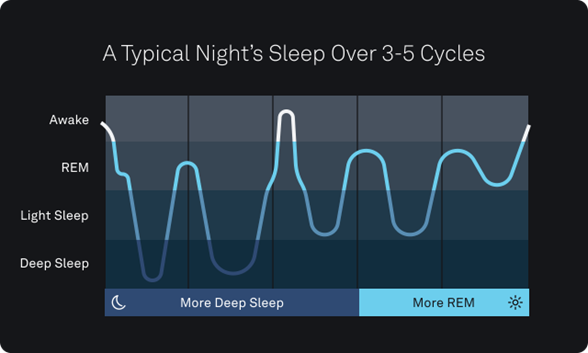
Source: Oura Team: What are the stages of sleep? (Published February 18,2020) https://ouraring.com/blog/sleep-stages/#:~:text=In%20general%2C%20each%20cycle%20moves,to%20skip%20deep%20sleep%20altogether.
As we age, sleep quality declines.
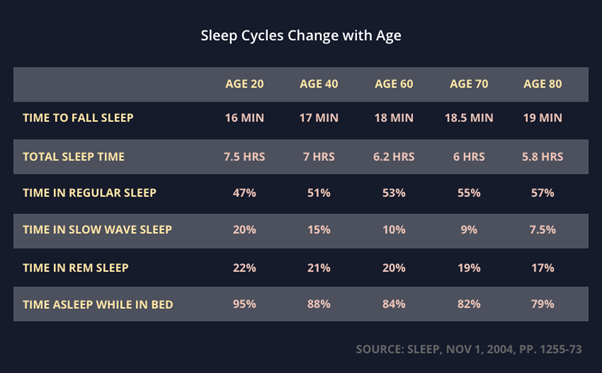
Source: https://sleepspace.com/what-are-delta-waves/
In adults, slow-wave sleep decreases by about 2% per decade of age. In men, it may no longer be present by the age of 60. Women maintain slow-wave sleep later into life which may account for men being 54% more likely to develop MND6, and 150% more likely to develop Parkinson’s7 than women.
Further reading: Fast Asleep by Michael Moseley (2020)
by Robyn Rix
References:
- Ben-Shlomo Y, Whitehead AS, Smith GD: Parkinson’s, Alzheimer’s, and motor neurone disease BMJ 1996; 312:724 doi: https://doi.org/10.1136/bmj.312.7033.724 (Published 23 March 1996)
- Benveniste H, Liu X, Koundal S, Sanggaard S, Lee H, Wardlaw J: The Glymphatic System and Waste Clearance with Brain Aging: A Review. Gerontology 2019; 65:106-119. doi: 10.1159/000490349
- Jessen NA, Munk ASF, Lundgaard I, Nedergaard M: The Glymphatic System – A Beginner’s Guide. Neurochem Res. 2015 Dec; 40(12): 2583–2599. doi: 10.1007/s11064-015-1581-6
- How To Sleep Well with Michael Mosley (2022), directed by Dani Carpanen, produced by Jon Willers, executive produced by Natalie Humphreys. SBS June 2022
- Wright D: On your back? Side? Face-down? Mice show how we sleep may trigger or protect our brain from diseases like ALS. (Published: May 27, 2022 1.07pm AEST) https://theconversation.com/on-your-back-side-face-down-mice-show-how-we-sleep-may-trigger-or-protect-our-brain-from-diseases-like-als-181954
- Alonso, A et al. “Incidence and lifetime risk of motor neuron disease in the United Kingdom: a population-based study.” European journal of neurology 16,6 (2009): 745-51. doi:10.1111/j.1468-1331.2009.02586.x
- Wooten GF, Currie LJ, Bovbjerg VE, et al. Are men at greater risk for Parkinson’s disease than women? Journal of Neurology, Neurosurgery & Psychiatry 2004;75:637-639.

Comments are closed.