Pilates and pelvic floor dysfunction (PFD)
Pelvic Floor Dysfunction (PFD) is most commonly linked to the symptom of Stress Urinary Incontinence (SUI). SUI is the leaking of urine during exercise, coughing or laughing and is a sign that the body’s stabilising system is breaking down. SUI can also be at the root of pain in the lower back, hip and buttocks, pubic symphysis, or sacroiliac joints, due to the extensive interconnection of fascia between these key muscle groups. We must also be mindful of urge incontinence, that occurs with urgency and timing and the individual may be caught short, so to speak!
Incontinence is very common in women and is now more reported in men. The Australian Bureau of Statistics states that up to 65% of women and 35% of men suffer symptoms of urinary or faecal incontinence. Most do not seek treatment because they are embarrassed or they assume it’s normal because they have had children, or they believe it is an inevitable part of ageing. This reluctance to disclose may mean that weare instructing some clients in a way that is not helping and may even be exacerbating, their condition.
How do we improve our Pilates practice?
Pelvic Health History:
As part of our initial assessment, we need to ask clients about their pelvic health, including any symptoms of incontinence. For women, we need to ask about obstetric history, number of births, method of delivery and any complications/trauma during and after the birth. We also need to document any gynaecological surgical history and stage of menopause. For the men, we can ask about any prostate history. To assist in the client’s understanding, it is good to explain the inter-relatedness of PFD and incontinence, with pain in other areas of the body.
Refer out:
Encourage all women who have SUI, have recently given birth, or who consider they may have an issue, to get assessed by a qualified pelvic floor physiotherapist. A pelvic floor physiotherapist can also assist men. This therapist can then give advice on the best way to focus the pelvic floor during Pilates.
Appropriate interventions:
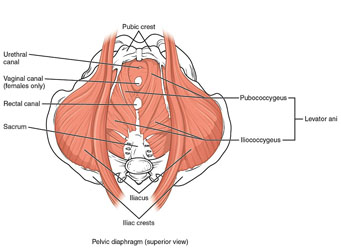
The solution to PFD is, very rarely to simply ‘do more Kegels’ or to ‘contract the TA and pelvic floor’ during active exercise. If pelvic floor muscles are hypertonic or the client’s breathing is dysfunctional, Kegels in isolation cannot help the problem. Dynamic core stability requires a balance of muscular support and a neuromuscular pathway appropriate to the movement being undertaken. All the abdominal muscles, spinal stabilisers, pelvic floor muscles and breathing diaphragm, need to work together in balance.
There is an optimal length/tension ratio for all muscles in the body, including the pelvic floor muscles. To generate a strong contraction when it is needed, pelvic floor muscles also need to be able to relax fully. It makes no sense to grip the gluts or flex the biceps all day – so why do we think that constantly contracting the pelvic floor or sucking the belly in, is any different? Constant or excessive tension in the pelvic floor muscles is just as dysfunctional as weak pelvic floor muscles.
Often we need to teach our clients to relax the pelvic floor, before they can learn to contract it correctly and to coordinate the action of the pelvic floor with the breath. If someone is already suffering from incontinence, they may be gripping there muscles and find it hard or frightening to relax them. A good first step is to try simple diaphragmatic breathing exercises to help your clients learn to coordinate the activity of the diaphragm, pelvic floor and abdominals.
Continuing Education:
Look into updating your training in pelvic floor/women’s health issues with a suitably qualified expert in the field. This may involve a workshop, training course or forming a mentor style relationship with a pelvic floor physiotherapist, that you can refer to and liaise with on your clients exercise program. Remember to seek out an educator/mentor who has both formal qualifications and clinical experience, so you are learning correct and current information and techniques.
Jen Guest and Chris Lavelle
PAA Committee

Comments are closed.